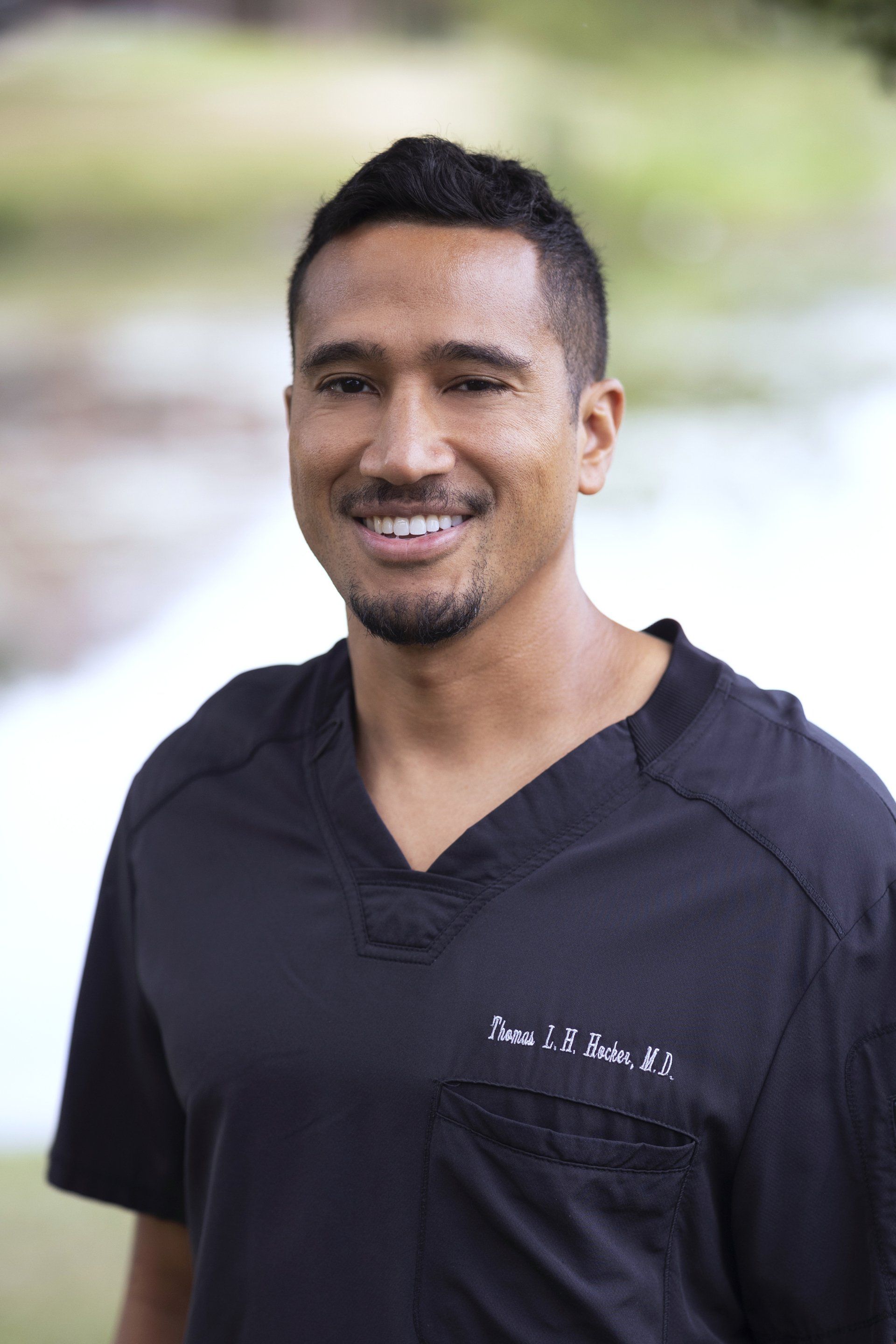
Thomas Hocker, M.D. is a triple board-certified dermatologist, dermatopathologist, and Mohs micrographic surgeon at Advanced Dermatologic Surgery in Overland Park, Kansas. He graduated from Yale University, where he studied biology, and received a Churchill Fellowship to study organic chemistry at Cambridge University in England. He attended Harvard Medical School, where he conducted melanoma research under Dr. Hensin Tsao, a world leader in melanoma genetics.
Dr. Hocker completed his internship at Santa Clara Valley Medical Center (Stanford-affiliated), followed by dermatology residency at Mayo Clinic. He pursued subspecialty training with a dermatopathology fellowship at the University of Michigan—home to one of the world's largest melanoma specialty centers—where he developed expertise in rare tumors. He then completed a second fellowship in Mohs micrographic surgery and facial reconstruction at Mayo Clinic under Dr. Clark Otley, receiving specialized transplant dermatology training.
Dr. Hocker has performed over 23,000 Mohs surgery cases and serves as founding division chief of dermatologic surgery at the University of Missouri-Kansas City and University Health. He is an active member of the International Transplant Skin Cancer Collaborative (ITSCC) and will be a key lecturer at the 2026 American College of Mohs Surgery national meeting.
He has been recognized as a Castle Connolly Top Doctor (2024, 2025) and received the Ingram's Top Doctor Award in 2025.