Mohs vs. Image-Guided Superficial Radiation Therapy (IGSRT): Why Surgery Still Leads for Most Non-Melanoma Skin Cancers
Mohs remains the gold-standard, guideline-preferred option for skin cancer patients.
Short answer: When a patient is a reasonable surgical candidate, Mohs micrographic surgery remains the guideline-preferred, margin-controlled, tissue-sparing treatment with the strongest long-term cure data for basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC). IGSRT can be useful when surgery isn’t appropriate, but its evidence base is newer, shorter-term, and lacks histologic margin control. (Medscape)
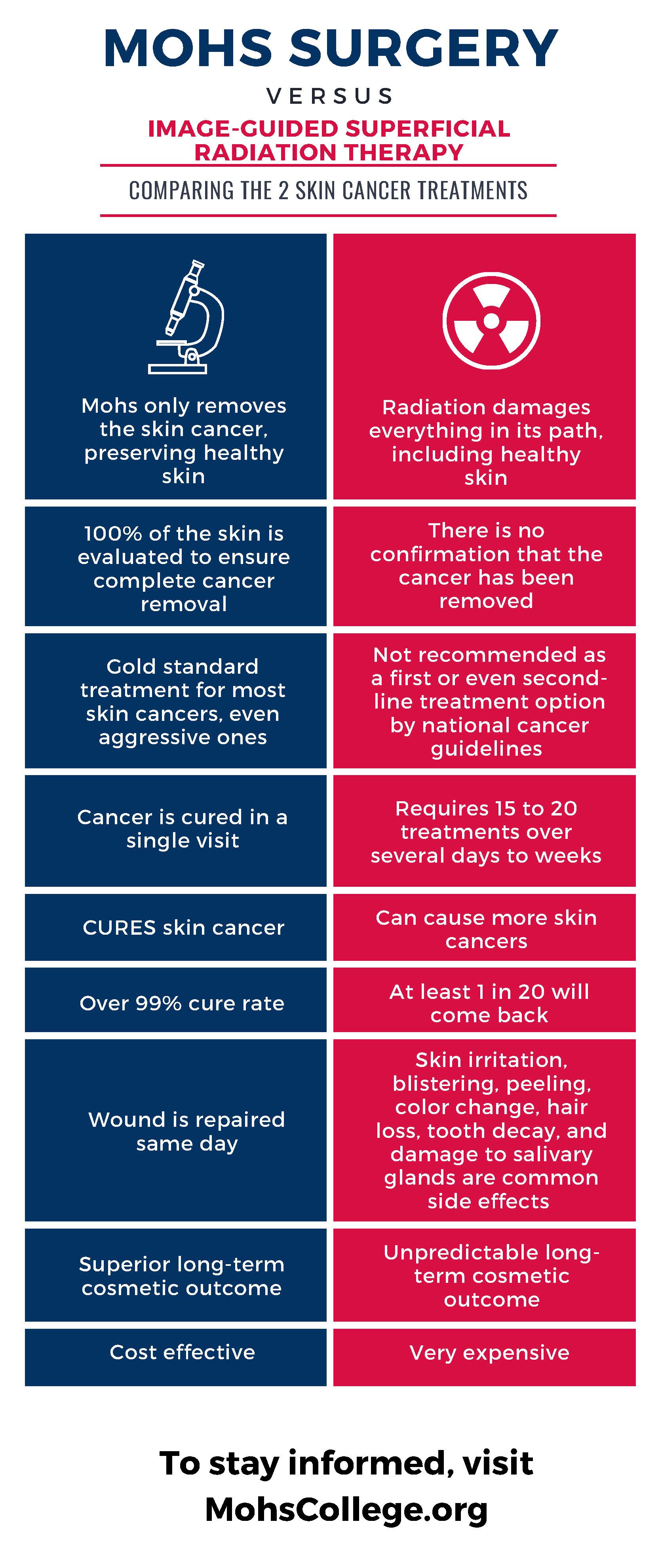
1) Mohs gives you real-time, 100% margin assessment
Mohs removes the cancer in thin layers and examines all peripheral and deep margins immediately, repeating until clear—so you know the tumor is out before you leave. Radiation (including IGSRT) cannot provide histologic margin confirmation at the time of treatment. That fundamental difference is why surgery is the preferred approach in major guidelines for most BCC/cSCC. (Medscape)
2) Best long-term cure rates (with 5-year outcomes)
Mohs consistently reports excellent 5-year control, often cited around ~2–3% overall recurrence for high-risk BCC cohorts, with higher—but still favorable—results in recurrent tumors. These are long-horizon data that matter in cancer care. (Medical Journals) By contrast, supportive IGSRT studies are retrospective and typically report shorter follow-up (often 2–4 years). Several recent series report low early recurrence, but the data are still maturing and may include selection and industry-affiliation biases. Short-term “superiority” claims versus Mohs at 2 years don’t replace 5-year histology-verified outcomes. (PMC)
3) Tissue-sparing + immediate reconstruction
Because Mohs removes only what is cancer while confirming clear margins, it maximizes healthy-tissue preservation—crucial on the eyelids, nose, lips, ears, and hands—and allows same-day reconstruction by the treating surgeon. Radiation can yield good cosmetic results for select lesions, but there’s no immediate histologic endpoint, and late skin changes (atrophy, telangiectasias, pigment changes) can occur. Guidelines continue to favor surgery for cosmetically and functionally critical sites when feasible. (Medscape)
4) Fewer visits, faster resolution
Mohs is typically a single-day outpatient procedure. IGSRT requires many fractions (commonly over several weeks) to deliver a curative dose. For busy patients—or tumors needing a timely, definitive margin-controlled result—one day often beats dozens of visits. (ASTRO’s practice guideline outlines definitive RT fractionation across 10–30+ sessions.) (ASTRO)
5) Where IGSRT fits (and where it doesn’t)
Radiation (including IGSRT) is appropriate for patients who cannot or should not undergo surgery, or for specific anatomic/clinical scenarios at the clinician’s discretion. Even radiation-oncology guidance frames RT as a good option when surgery isn’t ideal. Conversely, RT is generally avoided in certain genetic radiosensitivity syndromes (e.g., Gorlin), in previously irradiated fields, in some connective-tissue diseases, and younger patients due to late effects and second-cancer risk. (ASTRO)
6) What do major guidelines say right now?
NCCN & dermatology guidance: For most localized BCC/cSCC, surgery—preferably with comprehensive intraoperative margin control (i.e., Mohs) in high-risk settings—is the preferred curative modality. RT is a reasonable alternative when surgery is contraindicated or unsuitable. (Medscape)
ASTRO (radiation oncology) guideline: Defines when RT is appropriate, typical doses/fractionation, and cautions about patient selection—reinforcing RT as one of several tools, not the default first-line when surgery is feasible. (ASTRO)
Coverage climate: Some Medicare contractors have proposed limited-coverage LCDs and scrutiny around SRT/IGSRT utilization and daily image guidance—highlighting ongoing debate about appropriate use and billing. (CMS)
Bottom line
If a patient can safely have surgery, Mohs remains the gold-standard, guideline-preferred option for most BCC and cSCC because it proves clearance at the time of treatment, preserves tissue, and has long-term cure data. IGSRT is a valuable tool when surgery isn’t appropriate or is declined—but its evidence base is still catching up and it does not offer histologic margin control. (Medscape)
Medical note: Treatment should always be individualized by a board-certified dermatologist (often in collaboration with radiation oncology and other specialists). This article is educational and not a substitute for medical advice.
Selected references: NCCN and AAD guidance on BCC/cSCC; ASTRO skin cancer RT guideline; long-term Mohs outcomes; contemporary IGSRT series and reviews. (NCCN)